Accountable Health Communities Model
Accountable Health Communities Model
Did you know that where people are born, grow, work, and live directly impacts their health and well-being? These factors are known as health-related social needs or social determinants of health, and include things like access to food, housing, transportation and utilities.
Consider this situation: you have been recently diagnosed with a condition that requires adjustments to your diet, new medication, and regular checkups. You have every intention to follow the steps your doctor has suggested to you but run into a handful of challenges:
-
- You live in an area without a grocery store that is within walking distance, which makes it challenging to add the foods your doctor has suggested that will help you manage your condition.
- Your car hasn’t been working for months, and you don’t have enough money to have it fixed. This makes it challenging to make it to your checkups and difficult to pick up your prescriptions.
- Your new medication must stay cold to work well, but your utilities are shut off regularly because you are faced with the choice to pay for your rent or utilities.
You visit your doctor for a checkup, and your doctor asks how you’ve been feeling since your last appointment. You share your challenges, and your doctor listens with concern. Without knowing the full picture, including your housing, transportation, and food access needs, it’s hard for your doctor to offer the right support. That’s where screening for social needs can make a real difference.
Accountable Health Communities
Situations like this are why the Centers for Medicare and Medicaid (CMS) awarded Health Net of West Michigan and 27 other organizations across the United States funding to implement the Accountable Health Communities Model. The work spanned the period of2017 to 2022 and laid the foundation for collaborative efforts to screen for health-related social needs, build robust referral processes, and improve resource navigation practices.
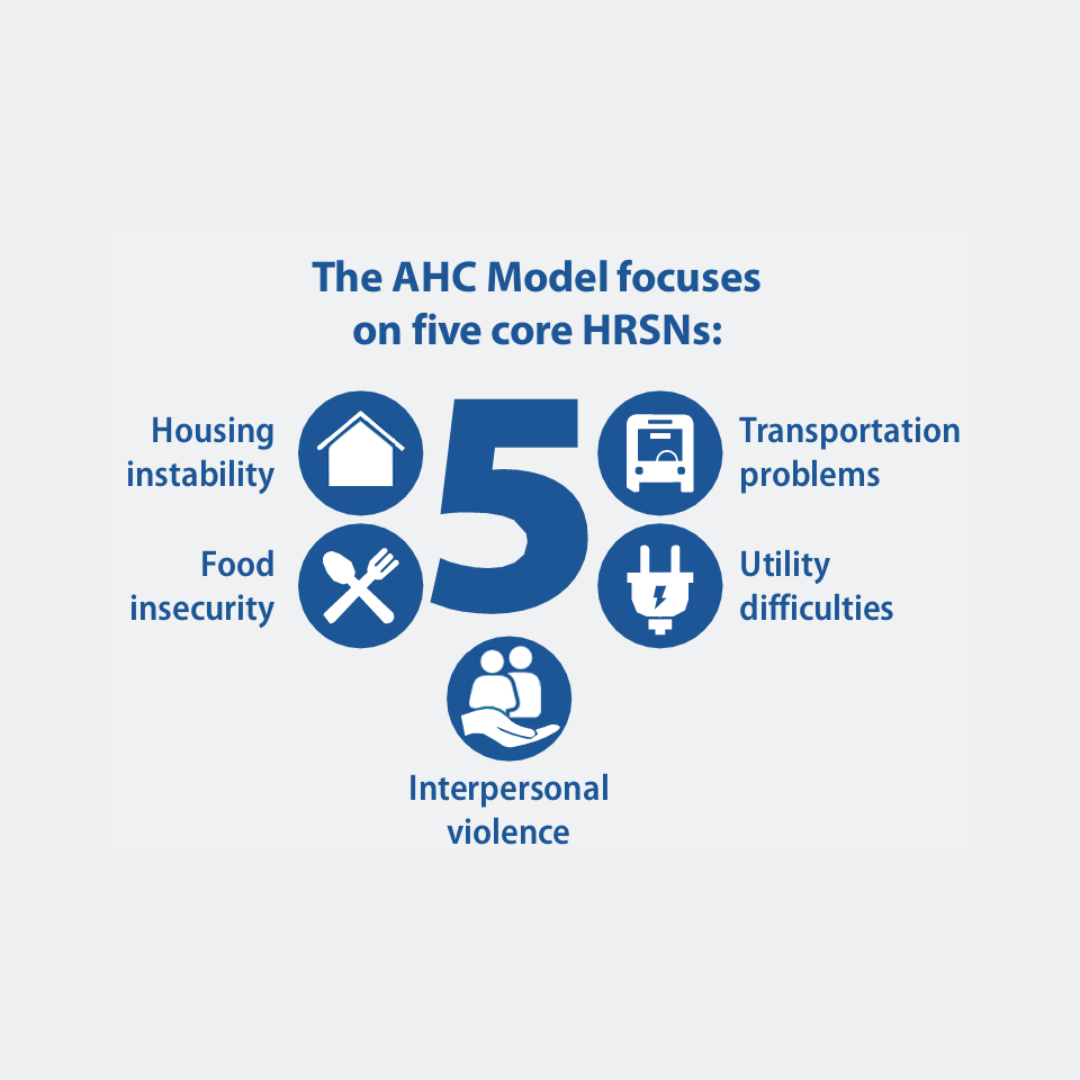
Throughout the project, the focus areas for screening included:
-
- Housing instability
- Utility needs
- Food insecurity
- Transportation
- Interpersonal safety
(To learn why these areas were chosen as the primary focus areas for screening click here.)
Project Goals
Through screening, referral, and navigation services the project aimed to achieve the following goals:
-
-
- Helping Medicare and Medicaid beneficiaries with unmet health-related social needs to connect with community resources through screening, referral, and navigation services.
- Optimize community capacity to address health-related social needs through quality improvement, data-driven decision-making, and coordination and alignment of community-based resources.
- Reduce inpatient and outpatient healthcare use and total cost by addressing unmet health-related social needs through referral and connection to community services.
-
Impact of Community Engagement
Read the case study about how Health Net implemented community input and engaged with our Community Advisors throughout the project.
Outcomes and Lessons Learned
Outcomes from the national project can be found here:
A full summary of the initiative can be viewed here:
The Accountable Health Communities Model highlighted how addressing health-related social needs directly supports the health and well-being of our community. At Health Net of West Michigan, we’re proud to carry these lessons forward and continue working toward a healthier, more connected community.